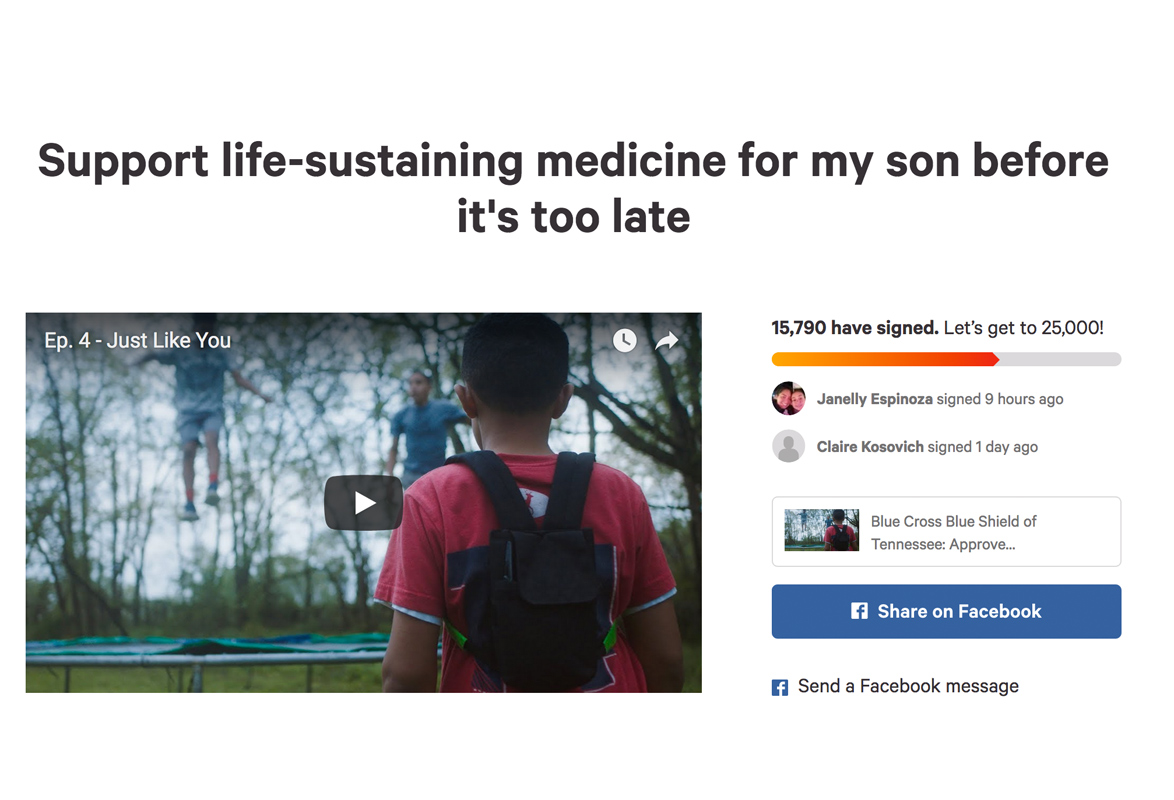
I never expected
over 15,000 signatures on our Change.org petition and all of the support in our challenge to Blue Cross.
Many of you have received a response from BCBST regarding your just complaints about their Idursulfase policy and their retroactive denials for Case’s coverage over the last 18 months.
While I had hoped we would have made progress, I am still disappointed by reality.
After my article last month, the petition, and a well-researched news article that got buried, BCBST introduced a new Idursulfase policy on August 14, 2018, that continues to suffer from many of the same problems and does not account for treating many children with Hunter Syndrome. And while they apologized and alleged that any denials of Case’s coverage were because of “human error” which has now been corrected and is supposed to not occur again, I cry foul.
The denials we received were CORRECT under their policy then and their policy now. Unfortunately. It’s a bad policy.
I offered to meet or connect BCBST with actual experts in Hunter Syndrome, but they did not take me up on my offer. They did not discuss this new policy or how it might apply to kids like Case or the families we serve.
Delay or denial of treatment
Their newly adopted Prior Authorization requirement and the (old and new) Idursulfase policy will only result in some Hunter Syndrome patients not receiving treatment.
In other words, your child might have Hunter Syndrome, but in some cases, they’ll tell you that Idursulfase is not “medically necessary” or not “appropriate for your situation.” Let me explain.
In November 2016, BCBST partnered with MagellanRX Management (a PBM or pharmacy benefits manager). Magellan touts its expertise in managing specialty medications such as high cost enzyme replacement therapies that are used to treat conditions like Hunter Syndrome (MPS II) and other MPS conditions.
Immediately, Magellan and BCBST implemented Prior Authorization (PA) requirements for a much longer list of drugs than BCBST had ever required PA (above is Magellan’s 2016 list – note the conflation of Elaprase for Hunter (no S) Syndrome and Xenazine for Huntington’s disease – no experts here). As you can see, along with many other drugs that fall into the “high cost, high complexity, or high touch” categories, those PA requirements included drugs like Idursulfase or Elaprase, the only FDA-approved drug to treat Hunter Syndrome.
Genetic, enzyme-deficient diseases
Hunter Syndrome, like the other MPS disorders, and like many disorders treated by high cost specialty medications, are genetic disorders. Enzyme replacement therapies like Idursulfase are *ONLY* used to treat the specific disorder, since they are a form of the enzyme the body is missing because of the genetic defect. No other conditions are missing that specific enzyme.
A physician would not prescribe Idursulfase for a condition other than Hunter Syndrome.
Therefore, the only purpose for having a Prior Authorization requirement and a stricter medical policy is to restrict those who have Hunter Syndrome from possibly accessing Idursulfase as a treatment option.
SO why would BCBST do such a thing? And where did the policy come from?
The message BCBST sent many of you who complained on their Facebook was that they “look to the experts, including reputable health care organizations, along with [their] network providers here in Tennessee.” That would make you assume that they consult physicians with expertise in Hunter Syndrome, almost all of whom I know personally, or maybe Project Alive, the leading Hunter Syndrome research and advocacy foundation, or the National MPS Society, the leading MPS organization in the US, or something along those lines. Nope.
The policy above, adopted by BCBST on August 14, 2018, just like the prior one, did not come from experts in Hunter Syndrome or local physicians who treat patients with Hunter Syndrome.
It came from MagellanRX, their contracted Pharmacy Benefit Manager.
How do I know? Because almost the exact same policy, most of the criteria is word-for-word, was adopted by another insurer that uses MagellanRX (and left their logo on the policy). And it was adopted by them in October 2017, ten months before this new BCBST policy.
And that was just one other MagellanRX insurer I checked. But their medical policies also matched BCBST’s for the enzyme replacement therapy Naglazyme (galsulfase) for MPS VI and the gene therapy Luxturna. I’m not saying those policies are wrong, but let’s all acknowledge that a company without specific expertise in the diseases (as far as I can tell) is consulting some publications and then writing policy.
And then insurers are taking those drafts, but then telling us they are consulting experts to write those policies.
And then those policies are being spouted back to us as expertise – to us, who know the diseases, the treatments, the side effects, the pros, the cons, the patients, the research that hasn’t even made it to clinical trials, and the science better.
All that being said, the new BCBST / ModaHealth / MagellanRX / ??? Idursulfase policy still fails to acknowledge:
- Outcomes in most patients are improved the earlier treatment is started (not waiting until 16 months of age) and literature and physicians who treat these patients will tell you that.
- Most of those with Hunter Syndrome over age 5 cannot perform the 6-minute walk test (6-MWT) or spirometry (the test which gives percent predicted forced vital capacity) so they cannot create a baseline or show improvement on those tests ← This is Case and every other cognitively impaired child with Hunter Syndrome, 70% of patients.
So what happens when a patient over 5 newly enrolls in a BCBST plan? Or once they turn 5?
Who may not be able to access Idursulfase under a policy such as this?
- If you’re “lucky” enough to get diagnosed under 16 months old
- If you’re over 5 and can’t perform a 6-MWT or FVC
- If you’re under 5 and don’t show positive response to treatment [ding! ding! this one is correct]
- If you’re any age and develop antibodies and reactions (will they let your physician try to get them under control?)
I was told that Case was considered covered under the “stabilization” language of the policy. Is that because he is physically stable or cognitively stable? Or both? How would that apply to every other cognitively impaired child with Hunter Syndrome, most of whom are not on the clinical trial brain drug that is keeping Case cognitively stable?
And while the writing teacher in me clearly reads the “stabilization” language to modify 6-MWT or FVC (which Case can’t do), I would happily hear confirmation from BCBST that they interpret that language to mean stabilization or positive clinical response to therapy in some form (such as improved endurance, improved functional capacity, reduced spleen/liver volume, reduced urine GAG excretion, etc.) at whatever age (no above/below 5 thing – that age means nothing in this disease), similar to the United Healthcare policy. But if that’s how they’re going to apply it to Case, then the medical policy should clearly say so and be applicable to all other boys with Hunter Syndrome as well.